We want you to be aware as possible of the costs and benefits of reporting through us – we don’t want you paying for something with no ROI, but we want you to benefit from reporting as much as possible.
To that end, Graphium HealthTM offers a deeper analysis for your specific Tax ID number.
The process goes like this:
- You setup a HARP account for your TIN (instructions to follow)
- We’ll then send you a request to access your new HARP account
- We’ll review your TIN’s data, and
- We’ll provide you a TIN-specific cost analysis.
First, we will look at each provider in your TIN to see whether they are individual or group eligible. Then we’ll examine your TIN’s estimated Medicare charges in the most recent 12-month period that CMS has available. What that allows us to do next is combine how many cases you do per year, how many providers you have, what the QCDR registration cost is per provider, the per-case cost to do this data collection and analysis process, and how that compares to how much money you can get on the upside. We will give you a break-even number to tell you what percentage you would need to hit to simply recuperate the cost of reporting through Graphium Health, and then we can tell how much of a positive adjustment you can potentially expect through successful QPP participation in 2019.
If you are interested, you will first need to create what is called a HARP account, which CMS says will only take 5-15 minutes. Use the following steps:
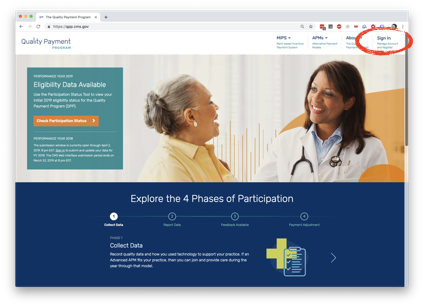
- Go the QPP Website: https://qpp.cms.gov/
- Click “Sign In” in the top-right corner (circled above)
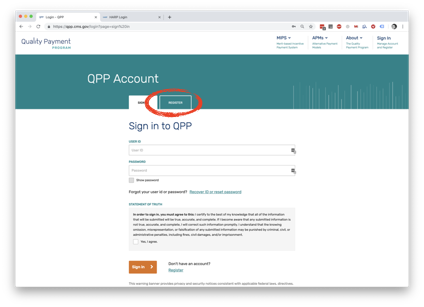
3. Click on the right tab titled “Register” (circled here)
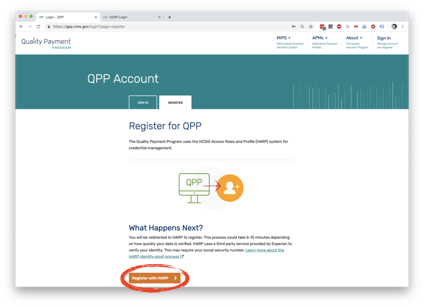
4. Then at the bottom of the tab, click “Register with HARP” (again- circled)
5. This will take you to the site pictured here, where you will start entering in information for your Tax ID number. They will validate your identity and then create an account for you.
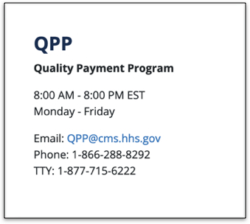
If you have any trouble at all registering for a HARP Account, you can use this contact information for the Quality Payment Program: