
CMS doesn’t call it MACRA, they call it the Quality Payment Program (QPP). We encourage everyone to visit the CMS QPP Website, where everything you need to know about MACRA should be available.
PENALTY vs BONUS
For 2019 both the penalty and the bonus increased to -7% and +7%, respectively, although it is highly unlikely that any providers or groups will receive a full +7% bonus. The QPP is “budget neutral,” which means that any bonuses that are paid out come from the penalties assessed to MACRA eligible providers & groups.
One nuance here is that CMS makes available an additional $500 million pool to those who achieve a Composite Performance Score (CPS) of 80 or greater—which qualifies them as “Exceptional Performers.”
Penalties, on the other hand, are assessed to those eligible providers who receive a CPS lower than 30. The exact penalties and rewards adjustments are not made known until all data is submitted – most likely by the Fall of 2020. While most of the maximum bonuses will likely fall in the 5%-6% range, the chart below demonstrates the range of penalty-bonus for a hypothetical provider group with $300,000 in annual Medicare charges.
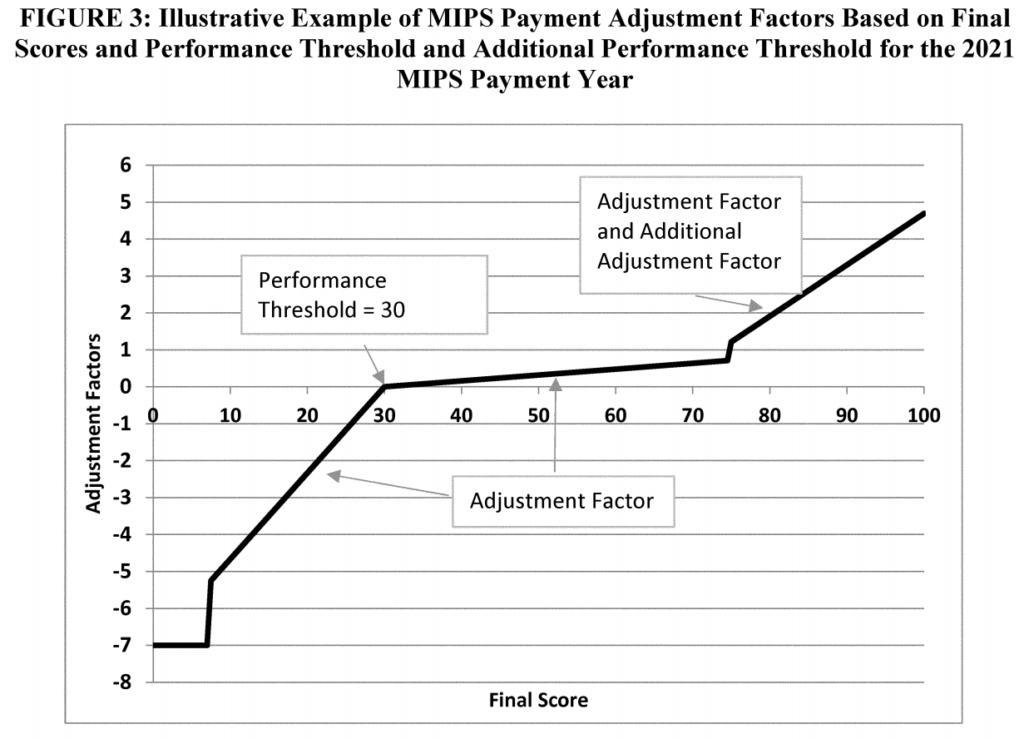
As you can see, the payment adjustment ranges from -$21,000 to +$21,000, which will be applied in 2021. Let’s dive a little deeper into the graph above, which comes from the Final Rule that was released by CMS in Fall of 2018. The Y axis represents the payment adjustment factor, which is a percentage. The X axis shows a range of CPS scores from 0-100.
WHAT COMPRISES THE CPS?
The CPS score is composed from 4 categories that are individually weighted to add up to a total potential score of 100. Those categories & weights are:
- Quality (70%)
- Improvement Activities (15%)
- Cost (15%)
- Promoting Interoperability (0%)
Quality
In this category, CMS will measure anesthesia provider performance across 6 different quality measures. You can report as many as you like (Graphium’s forms actually capture 7+), but CMS will only accept 6. Luckily, CMS will select the 6 measures on which providers perform the highest. Making up 70% of the final CPS score, Quality is significant, but not the only important category. As a reporting NPI or TIN, though, you will need to focus the most here —so we will devote an entire blog post on Quality Metrics soon.
Improvement Activities
If you reported with Graphium in 2018, you will remember that this category is based on an annual attestation of certain Improvement Activities. Graphium customers attest to 3 different improvement activities over a 90-day period.
Cost
Two years ago, this category was weighted at 0%. Then last year, the weight was raised to 10%, and this year it is weighed at 15%. Unfortunately, the cost here is a black box. No data needs to be submitted here, because CMS does that on their own.
Promoting Interoperability
The field of Anesthesia continues to receive hardship exemptions from this category, and so it is weighted at 0% of the overall CPS score, and no reporting is necessary. On the other hand, this category is on the radar, so it may be time to think about partnering with a company such as Graphium Health, who is known as the foremost integration specialist in the realm of Anesthesia software & technology tools.

