Introduction
In an effort to simplify MACRA reporting requirements for Eligible Providers (EPs), CMS provides a variety of reporting options to both incentivize data submission and penalize poor quality outcomes. The resulting complexity of these options may lead to confusion, frustration, and most importantly, missed opportunity. At Graphium Health, we strive everyday to provide clarity and answer questions as they arise. It has become abundantly clear to us that many anesthesia groups need to revisit the Individual vs Group reporting options in order to determine which one makes the most sense for them in 2018.
Three Categories of MACRA Payment Adjustments (Figure 1)
(1) Negative Payment Adjustment Factor (i.e. “MACRA Penalty”). The 2018 penalty has increased from -4.0% to -5.0%.
(2) Positive Payment Adjustment Factor. Of note, while the maximum projection had been estimated at 1.0%, the actual maximum for 2017 was 0.41%. This was due to both a much higher participation rate than initially projected (approximately 91% of all Eligible Providers reported in 2017) coupled with higher than anticipated scores. Recall that the total Negative Adjustment Factor fully funds this bonus category, such that the penalty and bonus are “budget neutral”.
(3) Exceptional Performer Adjustment. Just as in 2017, this will be an additional $500 million bonus pool of money CMS sets aside to be distributed to EPs with CPS > 70. Again of note, the maximum bonus for this category in 2017 was 1.61%.
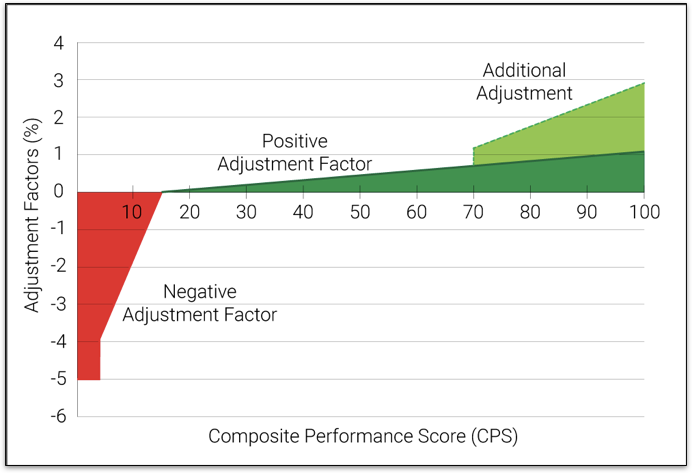
Figure 1: Qualitative view of the 3 different categories of MACRA payment adjustments. The actual values will vary and depend on participation levels for 2018.
Exempt Criteria – Definition
To further limit the reporting burden on low volume EPs, CMS has increased the “Exempt” thresholds for 2018. Specifically, the updated criteria include:
(1) Correct Eligible Provider type
(2) Enrolled in Medicare before January 1, 2018
(3) Medicare patients for clinician or practice > 200
(4) Allowed charges for clinician or practice > $90,000
Exempt Criteria – Individual vs Group
CMS applies the above criteria thresholds to BOTH the “individual” EP and to each of their TINs (i.e. “Groups”) based on the claims received from Sept 1 – August 31 of the preceding year. Many providers will find themselves BOTH “MIPS Exempt as an Individual” and “MIPS Included as a Group“.
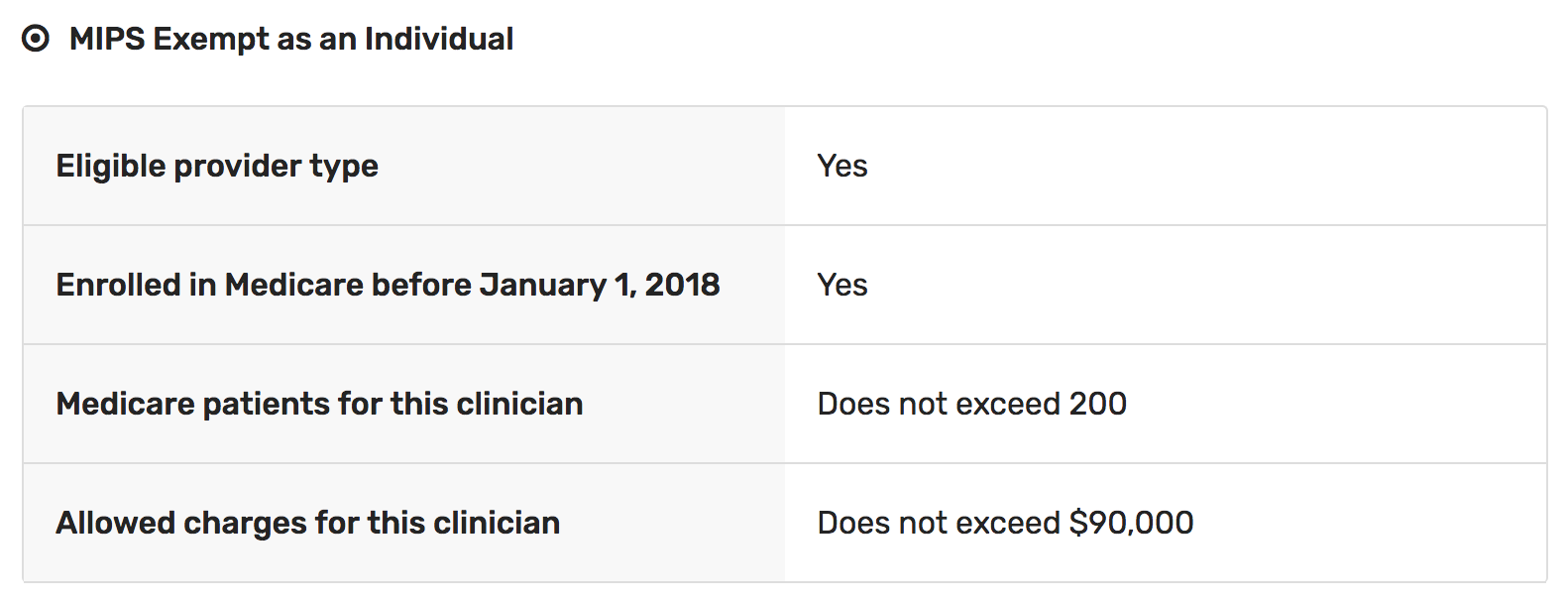
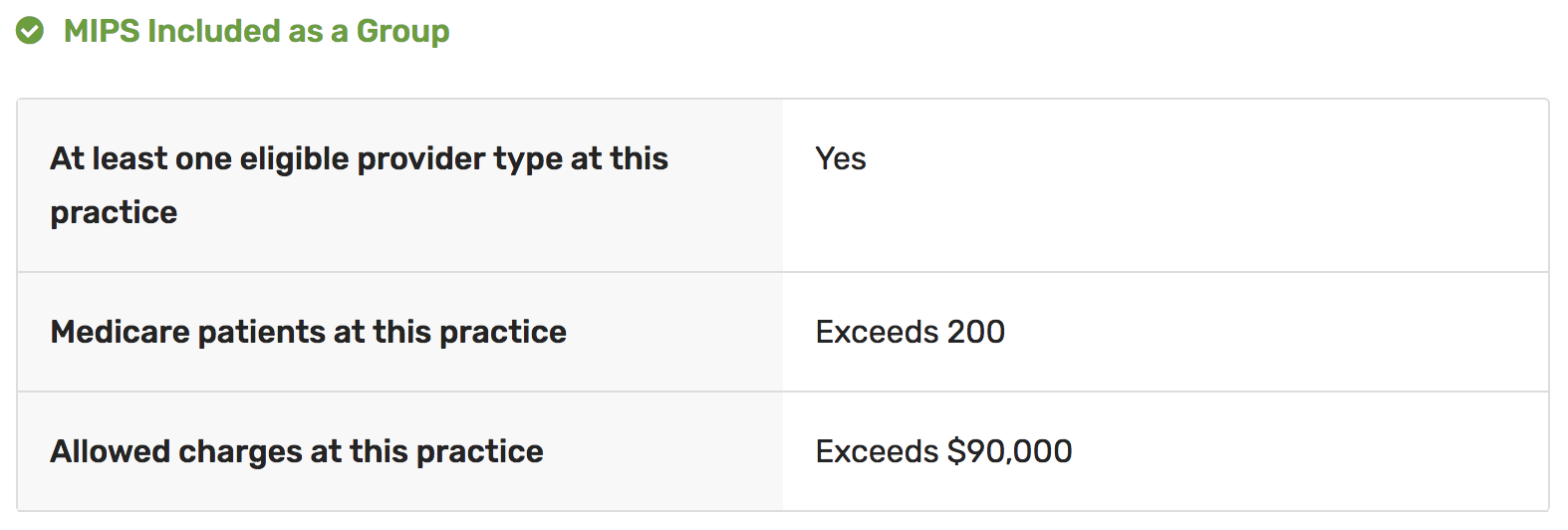
Figure 2: Results from CMS “Participation Status” website, showing how a single NPI is both “MIPS Exempt” and “MIPS Included” for the same TIN.
Consider an EP who bills under 3 different TINs. CMS evaluates the “Exempt” status of this EP for both Individual and Group reporting options – for each of the 3 TINs. This creates 6 different evaluations for the same single EP. The majority of anesthesia providers’ exempt status is far from cut and dry, and we recommend all providers check their NPIs for eligibility at: 2018 MACRA Participation Status
We estimate the 2018 thresholds have been raised so high for 2018 that almost all – if not all – of your providers will be classified as “MIPS Exempt as Individuals”. If you want them to participate in the 2 bonus categories above, you will need to opt for the “Group Reporting” option.
Individual vs Group Reporting
When CMS labels a provider as “MIPS Exempt”, they are exempt from both penalty and any bonus opportunity. If an “Exempt” provider chooses to submit quality data, they become a “Voluntary Submitter”, meaning CMS will still score their data and assign a final Composite Provider Score, but there will be no payment adjustment. No penalty. No bonus.
However, this very same provider is more than likely also labeled “MIPS Included as a Group”, meaning if you choose the “Group” reporting option, then this provider – as well as every provider in the group – will be eligible for both bonus and penalty, and in fact, each EP will share the same averaged CPS.
A Tale of 2 Anesthesia Groups
Let’s walk through two different examples. In both examples, there are 12 EPs who generate $500,000 in Medicare charges, and for simplicity, let’s assume their 2018 bonus potential is the same as the 2.02% bonus in 2017.
EXAMPLE 1: Equal Distribution of Clinical Caseload
This model assumes clinical caseload is equally distributed among all 12 members, and thus each EP is both “MIPS Exempt as an Individuals” and “MIPS Included as a Group”.
Option 1 – Individual Reporting:
(1) Each EP is viewed as a “Voluntary Submitter”
(2) Each EP would avoid the 5% penalty
(3) No EP would receive a Positive Payment Adjustment
(4) No EP would receive an Exceptional Performer Adjustment
(5) You can choose to not register any EPs with the QCDR
Option 2 – Group Reporting:
(1) Each EP shares the same CPS. A 2.02% max bonus on $500,000 in revenue amounts to a bonus of $10,100.
(2) Each of the 12 EPs in the group must register with the QCDR for a total required fee of $1,920 (12 * $160 registration fees).
In this example, we’d recommend Group Reporting option in which you spend $1,920 for the opportunity to receive $10,100, for a net of $8,180.
EXAMPLE 2: Unequal Distribution of Clinical Caseload
This model assumes an unequal division of labor in which PRN or part-time workers are being used. For purposes of illustration, let’s assume 2 of the 12 providers perform 90% of the Medicare work and are thus both “MIPS Included as an Individual” and “MIPS Included as a Group”, while the remaining 10 EPs are the same as Example 1 (both “MIPS Exempt as an Individuals” and “MIPS Included as a Group”).
Option 1 – Individual Reporting:
(1) 10 EPs are viewed as “Voluntary Submitters”
(2) 10 EPs would avoid the 5% penalty
(3) 10 EPs would NOT receive a Positive Payment Adjustment
(4) 10 EPs would NOT receive an Exceptional Performer Adjustment
(5) 2 EPs would get individual Composite Performance Scores. A 2.02% max bonus on 90% of the $500,000 revenue amounts to $9,090 in bonus.
(6) You can choose to register only the 2 EPs eligible for a bonus at a cost of $320 (2 * $160 registration fee)
Option 2 – Group Reporting:
(1) Each EP shares the same CPS. A 2.02% max bonus on 100% of the $500,000 in revenue amounts to a bonus of $10,100.
(2) Each of the 12 EPs in the group must register with the QCDR for a total required fee of $1,920 (12 * $160 registration fees).
In this example, the Individual Reporting option would cost $320 for the opportunity to receive $9,090, for a net of $8,770. Interestingly, had the Group Reporting option been chosen, this group would still net $8,180.
Bottom Line
These scenarios illustrate how the choice between Individual or Group Reporting depends on the distribution of Medicare revenue among your EPs. It’s also important to highlight how only the Individual Reporting option risks earning $0 in bonus, and even when selected, yielded only a nominal increase in positive payment adjustment over the Group Reporting option.
Perhaps some groups have unique dynamics that make the Individual Reporting option more advantageous, such as having more heavily loaded PRN labor mixed with fewer full time EPs. We suspect, however, that these groups are few and far between. If you are unable to analyze your group’s Medicare billing data per provider, it is our opinion that you should strongly consider the Group Reporting optionas your likely best reporting option for 2018.
If you have any questions about your group’s current position, please don’t hesitate to reach out to our team.
The combined 2017 revenue swing from failed MACRA reporting (i.e. CPS = 0) to perfect MACRA reporting (i.e. CPS = 100) amounted to 6.02% of Medicare billing, and this should increase further for the 2018 reporting year.
It’s very likely your group needs to convert to Group Reporting for 2018 to ensure you don’t miss out on the bonus adjustments.

