2017 preliminary MACRA Scores have arrived!
While they will be finalized later this Summer, they’re worth reviewing to better understand what it means for anesthesiologists and CRNAs to be MACRA compliant. In this article, we break down the components of your individual score posted at CMS and explore just a few of the many caveats to consider.
MACRA compliance boils down to receiving a “Patient Safety/Quality Score” every year ranging from 0 to 100. It’s technically called the “Composite Performance Score” or “CPS”, and unless your practice was exempt, every Anesthesiologists and CRNAs received a score for 2017. In fact, if you billed under multiple Tax ID Numbers (TINs), then you may have received multiple scores. To help keep things straight, let’s walk through exactly what you see on CMS’s website and what it all means.
But first, recall 4 components make up your final CPS, including:
(1) Quality (60%)
For the Quality portion, a maximum of 6 quality measures may be reported, and these measures are either “MIPS” or “Non-MIPS” (also called “QCDR”) measures. Graphium reported 8 “QCDR” Measures, and CMS will select the 6 best measures, discarding the remaining 2. Because the Advancing Care Information section is waived for a majority of anesthesia providers, this section is actually worth 85% of your final CPS.
(2) Advancing Care Information (15%)
The Advancing Care Information portion will be waived by default for almost all Anesthesiologists and CRNAs, as they are classified as “Non-Patient Facing” providers. Pain specialists and Critical Care Medicine specialists will not have this same exemption.
(3) Improvement Activities (15%)
The Improvement Activities portion consists of simple attestations at the end of the year to questions asking how the collected data was used to improve patient outcomes.
(4) Cost (0%)
The Cost portion was waived entirely for all providers in 2017. (In 2018, it will compromise of 10% of your final score.)
So let’s get back to unwrapping your Preliminary Composite Performance Score!
STEP 1. Log in to your CMS Account at https://qpp.cms.gov
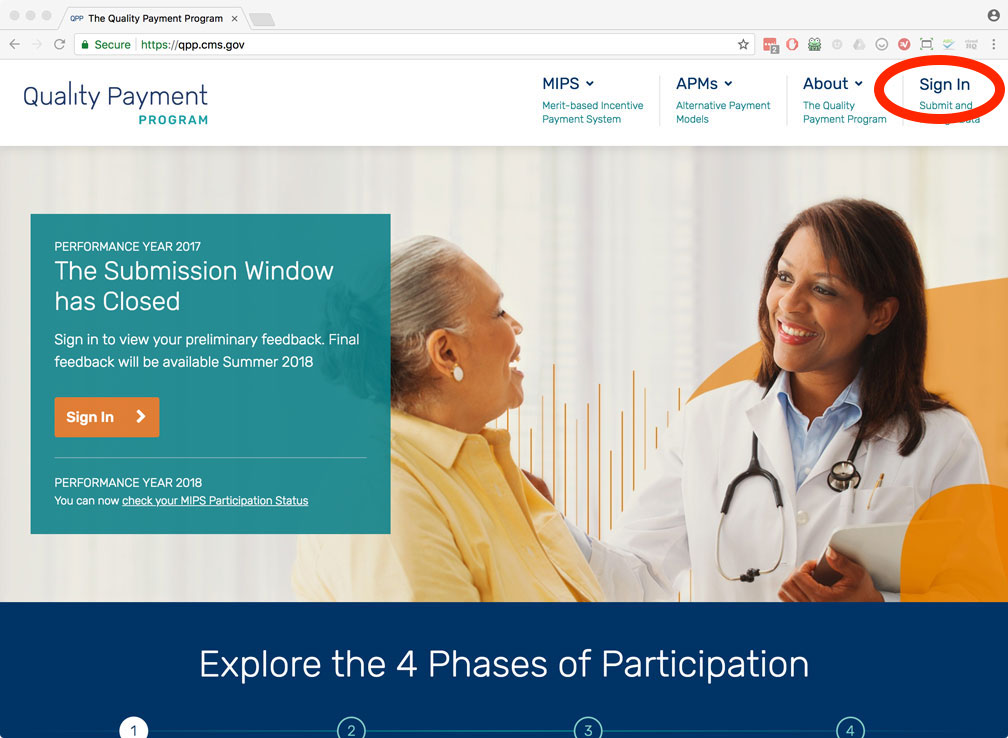
If you don’t already have an account, follow CMS instructions to create your Enterprise Identity Management credentials at https://portal.cms.gov or call 1-866-288-8292 and CMS will help you. Alternatively, you may need to contact your group administrator for more information on creating an account.
STEP 2. View Performance Feedback
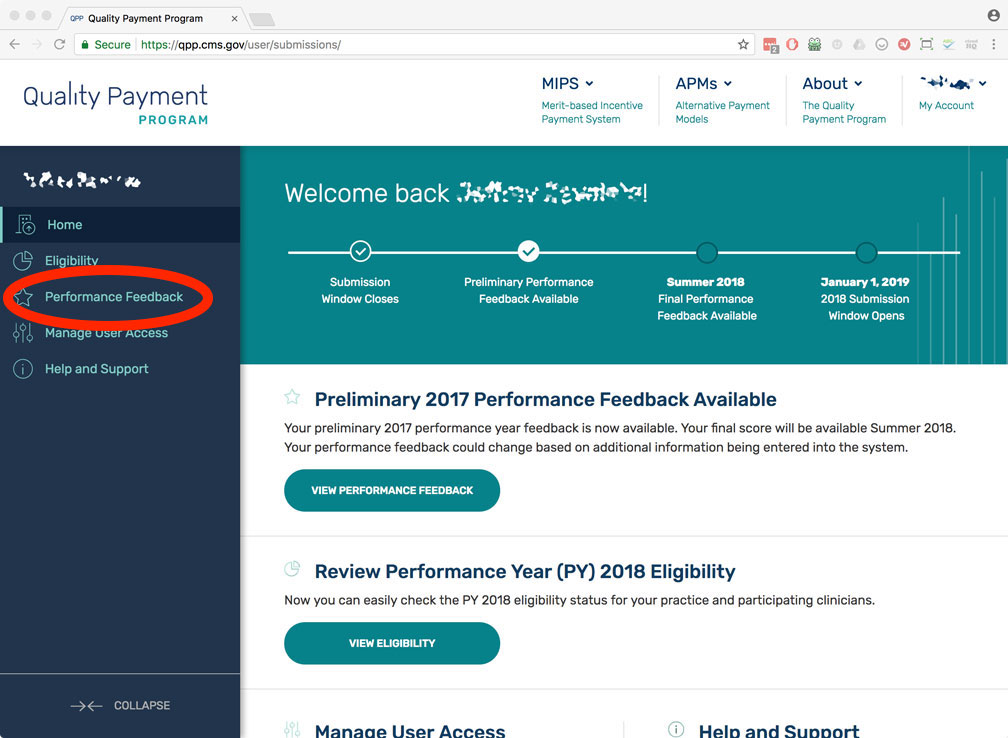
In the left menu bar, select “Performance Feedback”.
STEP 3. Preliminary Warning
CMS want you to understand that the scores currently presented are “Preliminary”. Nothing is final until “Summer 2018” which could be anytime very soon. We’ve watched these scores for the past several months and noticed them consistently climbing. So we suspect these scores will become “Final” sooner than later.
The specific “warnings” which pertain to anesthesia practices include:
(1) “Hardship Application status”
All “Non-Patient Facing” eligible providers are automatically exempt from the “Advancing Care Information” category. This includes Anesthesiologists and CRNAs. For most providers, this section accounts for 15% of your final CPS; however for anesthesiologists and CRNAs, this 15% is reduced to 0% and the “Quality” section is raised from 60% to 85% of your final score.
(2) “Any benchmark updates for Quality measures that have met minimum threshold criteria”
Each quality measure reported to CMS is either “Benchmarked” or “Non-Benchmarked”, meaning if there is enough nationally submitted data, then your individual performance may be “benchmarked” against the national average for a given specific quality measure. Importantly, a “Benchmarked” measure has a maximum score of 10 points, whereas a “Non-benchmarked” measure maxes at 3 points. Graphium submits the maximum 6 measures, and it’s our hope these measures will be classified as benchmarked, thereby raising the max potential cumulative score from 18 to 60 for the “Quality” portion of the CPS.
STEP 4. Select your Tax ID Number (i.e. Select your group practice)
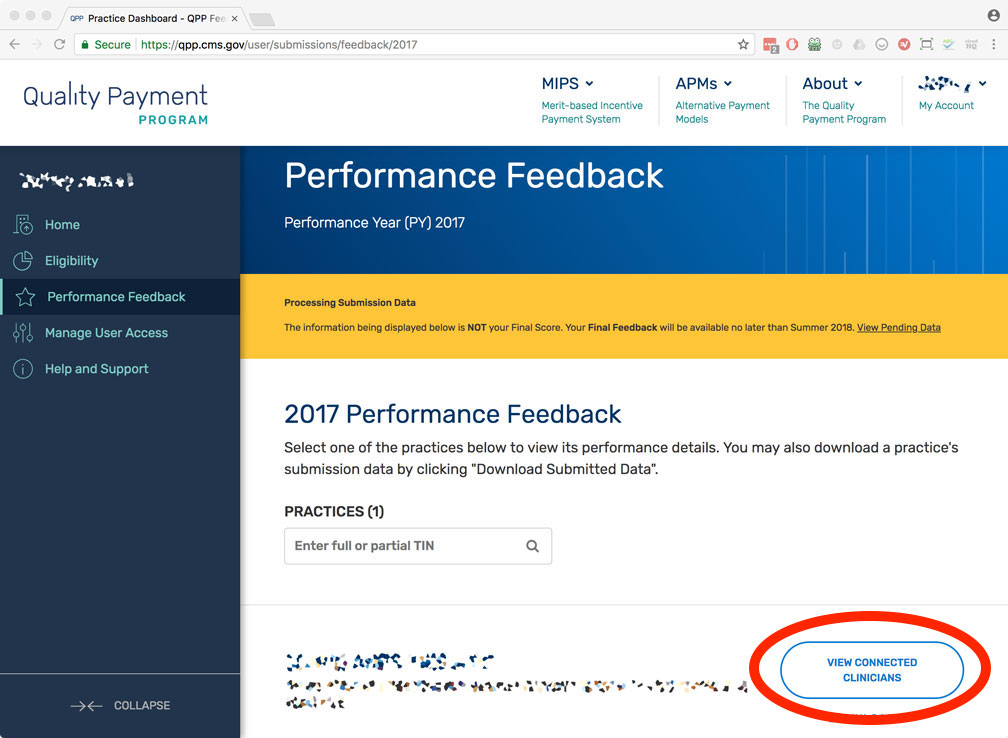
f you submitted claims under multiple TINs, then you may have received multiple Composite Performance Scores – one for each TIN you reported under.
STEP 5. Select your National Provider ID
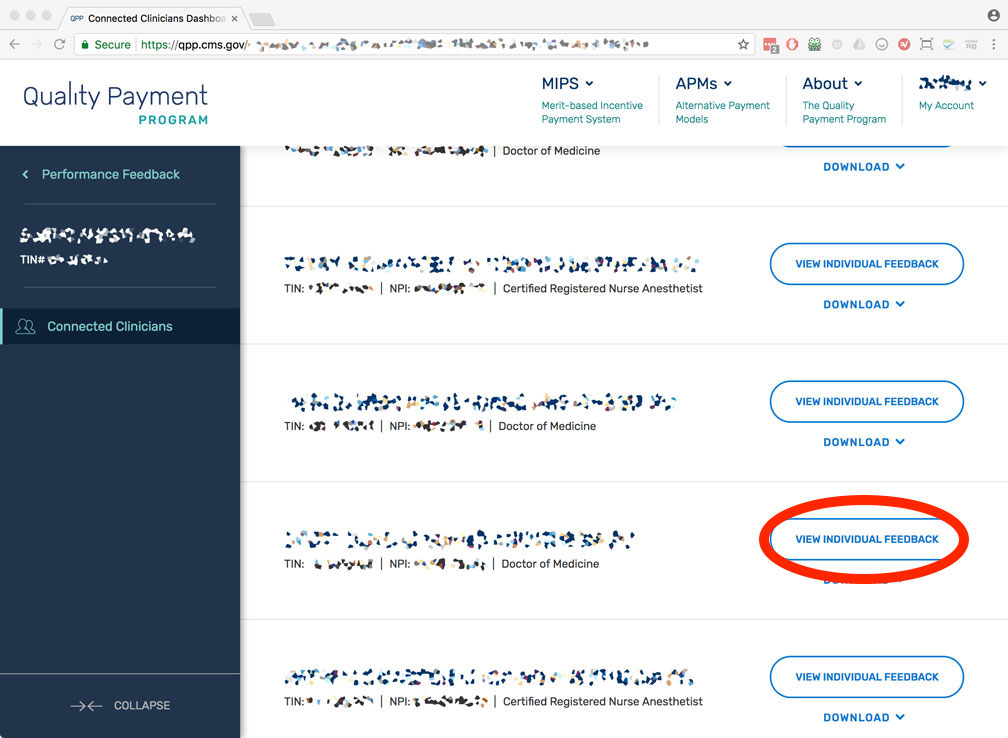
Once you’ve found your name, click on “View Individual Feedback
STEP 6. Provider Composite Performance Score
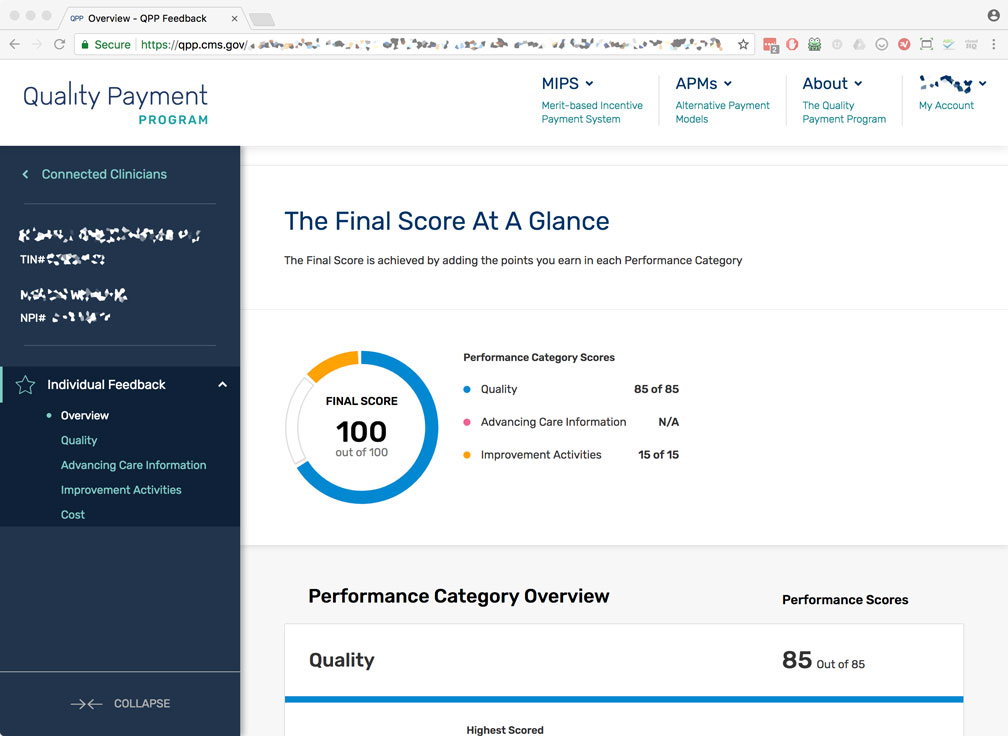
At last, you’ve found it! All of those forms submitted in 2017, and here you can finally see your “Preliminary” score. It will range from 0 to 100, and in this particular anesthesiologist’s case, they scored a perfect 100 points! Way to go!
Some observations:
(1) They received the full 85% available for the Quality portion.
(2) They received the full 15% available for the Improvement Activities.
(3) They will avoid the 4% penalty, applied in 2019.
(4) They will participate in the “Positive Payment Adjustment” which amounts to an additional 1% bonus.
(5) Because they exceeded the “Exceptional Performance” threshold of 70 pts, they will receive an additional portion of a $500 million pool of money set aside by CMS.
This particular group had Allowed Charges of $500,000 for over 1,700 Medicare patients, meaning if all providers performed as well, the group will see an additional income swing of $25,000, plus an as-of-yet undetermined portion of the $500 million bonus pool in 2019.
Let’s take a closer look at that Quality portion, as it’s the lion share of your final CPS.
STEP 7. Quality Overview
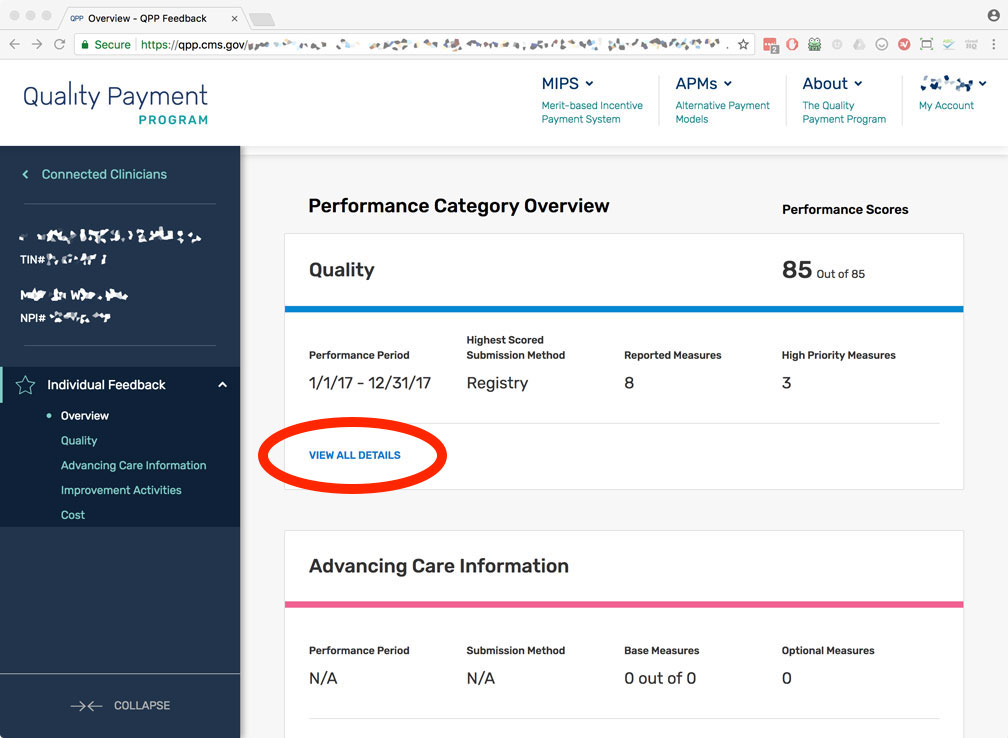
Click on “View All Details” to see more detail on the individual measures.
STEP 8. Quality Measures
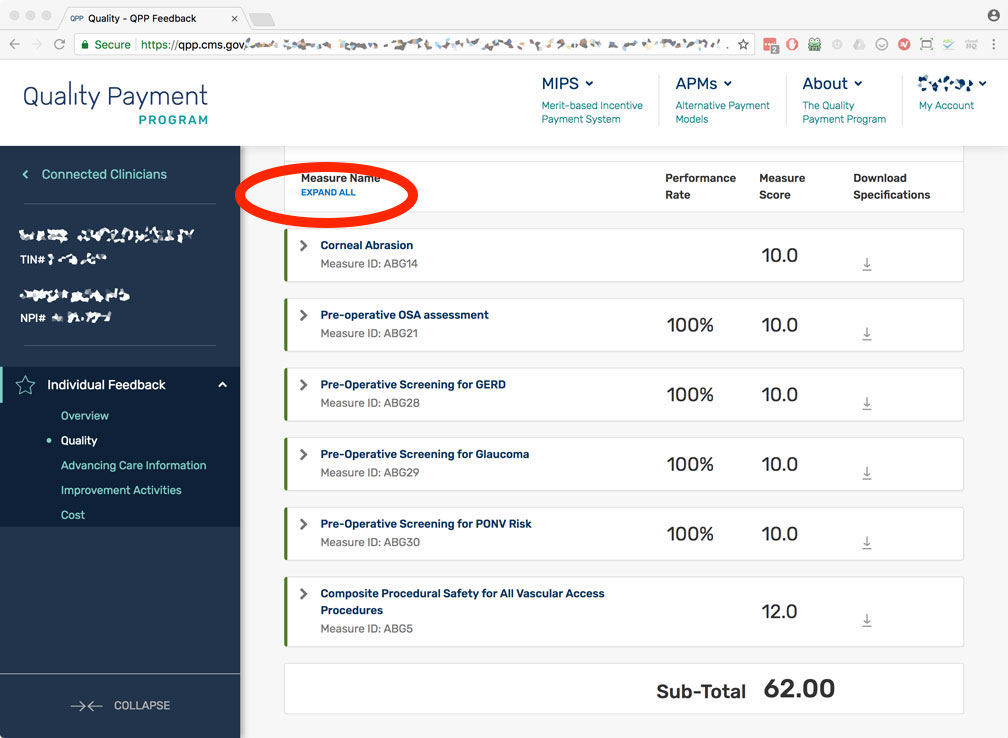
Here you’ll see you top 6 quality measures. Recall Graphium submitted a total of 8 measures, but only the top 6 are considered. This anesthesiologist had a “Performance Met” of 100% on 4 of the 6 measures, with the other 2 measures being “inverted” because they are bad outcomes. You can also see the number of points awarded to each measure. In this case, the max 10 points were applied to each measure, with the exception of the final measure receiving 2 additional bonus points, resulting in 12 points.
Let’s keep diving deeper and look at a individual quality measure. Click on “Expand All” to take a closer look.
STEP 9. Individual Quality Measure
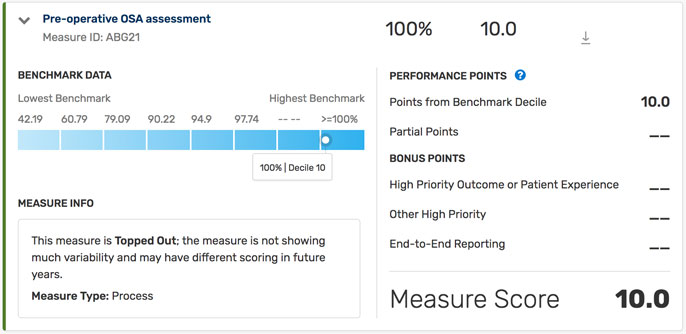
This is ABG Measure 21: Pre-Operative Assessment for OSA. First, notice it is a “benchmarked” measure, and as a result, we can see exactly how performances across the nation distribute in the blue graph. Each rectangle in the blue graph represents a 10-decile range, and exactly where your individual “Performance Met” percentage falls within this spectrum determines how many points you will receive for this measure. For example, if your “Performance Met” for this measure was reported as 97.5%, then you’d fall within the 7th-decile, and thus be awarded 7 points out of 10 possible. Importantly, regardless of the measure’s distribution, all 10 points will be awarded for performance met of 100%.
For many of these measures, the “Performance Met” percentage is “Topped Out”, meaning it was too good across all providers. CMS doesn’t like this. That is, if “everyone is performing at 100% for a given measure” then that measure is a poor differentiator in quality of care between providers. Don’t forget, the purpose of MACRA is to justify who to pay less in the name of quality. If everyone is “perfect”, then the measure needs to change. Thankfully, the measures for 2018 reporting have already been approved, but we expect changes in 2019.
You can also see that individual measures can earn “bonus points” if they are:
(1) High Priority Outcome or Patient Experience
(2) Other High Priority
(3) End-to-End Reporting
At Graphium Health, we are constantly interpreting which measures are “best” to report, and this depends on multiple factors, such as ease of data collection, maximum number of points available, and opportunity for bonus questions. There’s certainly inherent confusion with federal bureaucracies, but we remain confident in our measure selection for 2017 and 2018 MACRA reporting.
STEP 10. Quality Score Algorithm
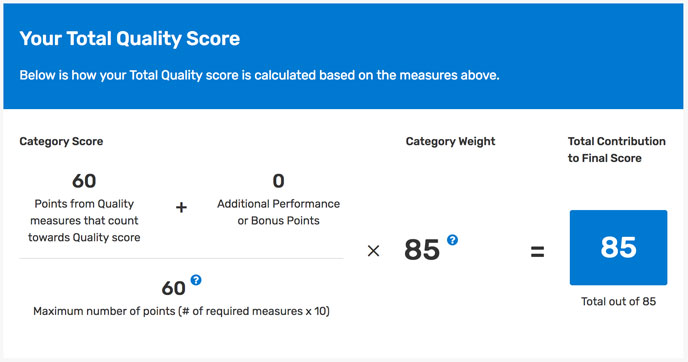
Because Anesthesiologists and CRNAs are considered “Non-Patient Facing”, the typical Quality portion of 60% is increased to 85%. From an algorithm standpoint, CMS evaluates each of 6 measures on a 10 point scale, with some additional points possible for special measures. The total from these 6 measures is then summated and capped at 60 points. In our example, the anesthesiologist scored 62 points, thus exceeding the maximum. CMS reduces this to “60 of 60”, and then multiples by 85 (or rather 85%). In this case, it amounts to the provider receiving the entire 85% for this portion, or 85 points.
STEP 11. Improvement Activities Overview
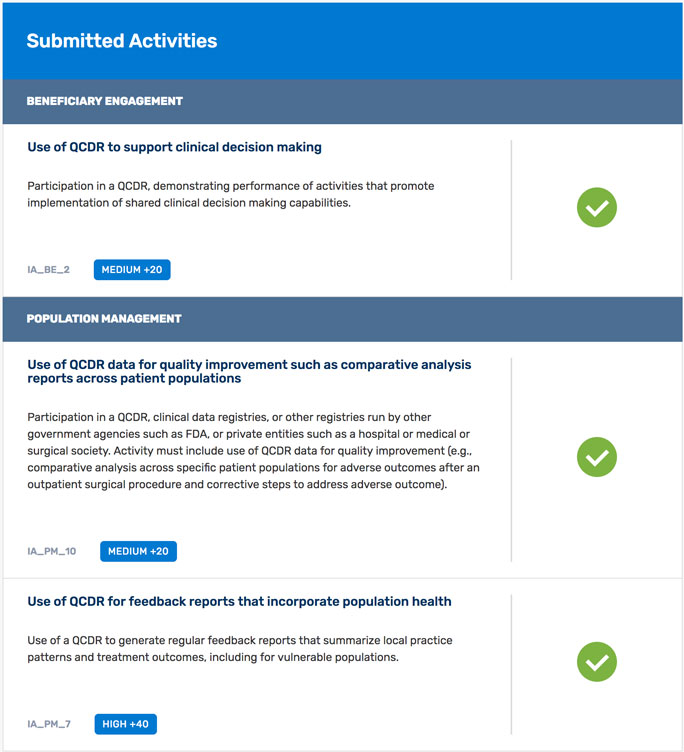
As mentioned in the introduction, the “Improvement Activities” portion consists of an end of the year attestation for your providers that describe how they use the data to improve outcomes. There are over 90 activities one may attest to, and each is worth a certain number of points. CMS sets a goal of 40 points for this portion to get full credit for this portion.
By successfully attesting to the 2 “medium” activities and 1 “high” activity described above, this anesthesiologist earned 80 total points, exceeding the 40 needed.
STEP 12. Improvement Activities Algorithm
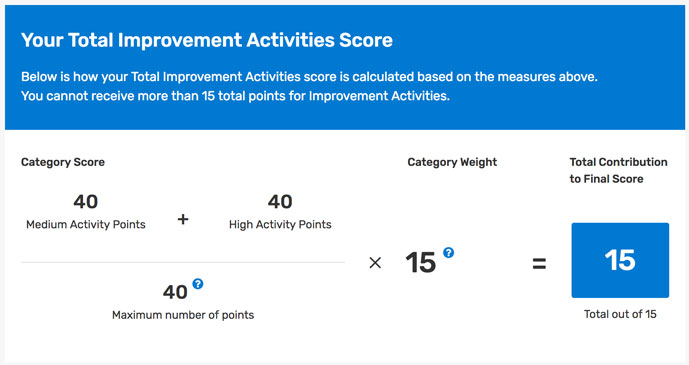
In true fashion, the math shown above simply isn’t mathematically accurate. [(40 +40) / 40 ] * 15 = 30, even in today’s new mental math world! Simply, CMS maxes this portion at 15 points total.
Conclusion
With our MACRA Ready™ service lines, Graphium Health intentionally reports more Quality measures than required and accommodates attestation of more Improvement Activities than needed as a “buffer”. It’s our way of mitigating the unknown and maximizing the chance of success. In this case, our reporting anesthesiologist received the maximum score of 100 points, ensuring:
(1) They avoid the 4% penalty
(2) They max their “Positive Payment Adjustment”
(3) Participate in the additional $500 million bonus pool

